Once you’ve determined who will lead and take part in the endovascular trauma program, the next step is to plan and secure the program’s physical resources and equipment.
One big question is whether or not to create a dedicated trauma hybrid room. Melanie Hoehn, MD, believes that hybrid rooms are useful but not essential to a successful endovascular trauma program.
“A hybrid room is nice if you have it, but in my opinion it’s not mandatory for setting up an endovascular trauma program,” Dr. Hoehn said. “It’s a very expensive undertaking, so if your institution does not have the resources to take that on, you can still implement a program with a portable C-arm as long as you get a machine of high enough quality and also put up all the other support systems.”
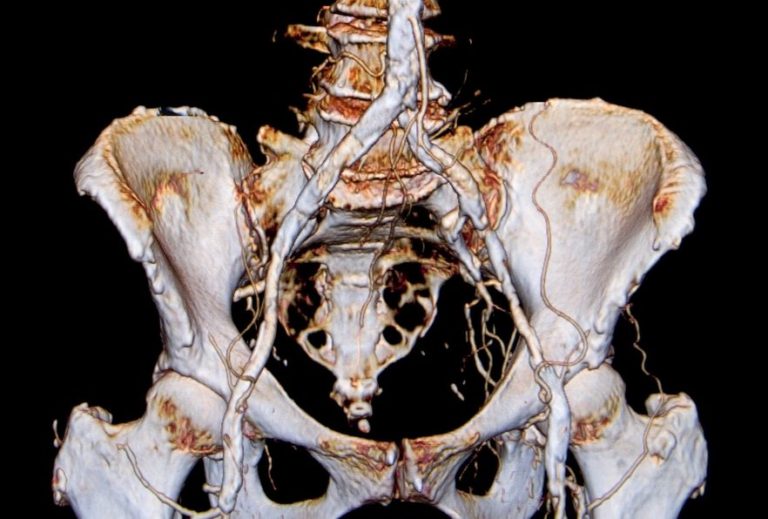
Imaging systems
What C-arm capabilities are essential? “It’s my opinion that any procedures you do in trauma tend to be in patients that are critically ill, and so the procedures tend to be relatively straightforward,” Dr. Hoehn said. In terms of imaging, that means the C-arm should enable basic to moderately complex procedures.
“The system you choose will vary a little based on the level of complexity of the procedures that you will be doing,” she said. “You definitely need one that runs vascular programs, and you’ll want…
This is Part II of How to Build an Endovascular Trauma Program at Your Hospital
Click below to jump to any section:
Intro – Trends and barriers
Part I – Creating the endovascular trauma team
Part II — Essential equipment and supplies
Part III — Training physician and nursing staff
Part IV — Ensuring quality and patient safety
…something that is going to give you a wide enough field-of-view that you can work on these cases.”
Key parameters include institutional resources and the unique makeup of your endovascular team. “Again, it’s going to depend a great deal on what your budget is, who is going to be using the system and what they will be using it for.”
Endovascular supplies
Core endovascular trauma supplies include all the basic wires, catheters and other items stocked in an endovascular room. You will also need a wide variety of stent grafts.
“So besides aortic stent grafts, you will want to have at least some thoracic devices available in-house,” Dr. Hoehn said. “In addition, it is very important to have some peripheral artery stent grafts on hand, in particular subclavian artery grafts. This would include some smaller covered stents.”
One way to ensure supply availability and control costs is to centralize endovascular services where possible. “At Shock, our trauma hybrid room was separate from our vascular room, so it was a challenge to centralize our equipment so it was readily available to the trauma team without someone having to go to the other side of the hospital,” Dr. Hoehn said. “We eventually had to duplicate some of the stock so that it was immediately available.”
Hybrid rooms: 3 keys to success
Juan Duchesne, MD, section chief of trauma and critical care at Tulane University School of Medicine, described his experience with the trauma hybrid suite at the Norman McSwain Trauma Center in New Orleans. He identified three keys to building and running a successful hybrid room.
1. Sufficient volume. “The main challenge is convincing administration that a hybrid room will benefit patients,” Dr. Duchesne said. “If you’re in an environment where you don’t see that much complex blunt trauma, it will be hard to convince administration to allocate all the resources for your trauma group.” The key is to demonstrate a sufficient volume of hypotensive polytrauma patients who would benefit from a hybrid room. “If you are a busy facility, you should be using the hybrid room an average of 2 to 5 times a month.”
2. Trauma surgery ownership. “It is extremely important that trauma surgeons are in control of these hybrid rooms,” he said. If another specialty is in charge of the room, it will often not be available when needed by an injured patient. “If trauma does not own the hybrid room, it will be used for many other procedures — procedures that will be indicated, but which will often not leave room for those patients with multiple comorbidities and vascular injuries. So it is extremely important that administration back up the trauma system on this point.”
3. Adequate specialty coverage. “You need to make sure that the interventional radiologists and vascular surgeons understand that there is a timeframe for responding to a trauma activation,” Dr. Duchesne said. Once the trauma activation call is placed, endovascular specialists need to be on site working with the patient within 30 minutes. “It is extremely important that the trauma group work together on this.”
Next section: Endovascular trauma: training physician and nursing staff