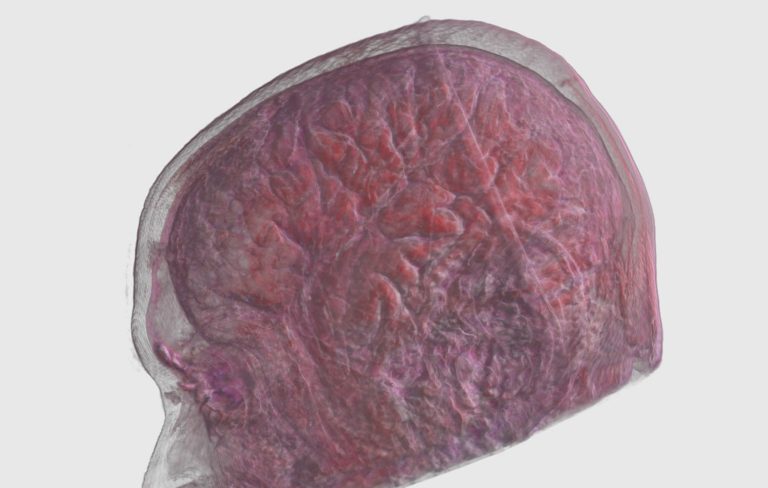
As the population ages, fall-related injuries will become an even bigger part of trauma care. A new study from NYU Langone Medical Center predicts that in the next 15 years, chronic subdural hemorrhage (SDH) will be the most common adult brain condition requiring surgery. The authors of the study question whether the U.S. will have enough neurosurgeons to handle this patient surge.
The research was published March 20 online in the Journal of Neurosurgery. The NYU team analyzed 12 years (2000 to 2012) of patient data from the U.S. Veterans Administration (VA). They also used data from Japan and Finland to create a mathematical model for SDH incidence in civilian populations. The model accounts for age, gender and alcohol consumption.
Results were summarized in an NYU press release:
- During the period studied, the SDH incidence rate for veterans was 79.4 cases per 100,000 individuals.
- Approximately 29% of these cases required surgical drainage.
- More than 70% of SDHs occurred in patients 65 years of age and older.
- By 2030, when up to 25% of the U.S. population will be older than 65, the incidence of chronic SDH will reach approximately 121.4 cases per 100,000 people in the VA population and 17.6 cases per 100,000 people in the general U.S. population.
“We have a very large population of elderly and the last of the 77 million baby boomers will have turned 65 by 2030,” said lead researcher Uzma Samadani, MD, PhD, chief of neurosurgery at New York Harbor Health Care System. “We can anticipate that 60,000 Americans per year will develop chronic SDHs.”
Challenging health problem
SDHs are more common in the elderly. Brain atrophy, anti-coagulant medications and the thinning of delicate bridging veins make older people more susceptible to subdural hemorrhage. SDHs are also more common in military veterans and in people with a history of alcohol abuse. According to data from the New York Harbor VA, SDH surgical patients have a significantly longer length of stay than other cranial surgery patients. They also require more intensive physical therapy and rehabilitation.
The NYU study suggests that healthcare providers, including trauma programs, will need to dedicate more resources to SDH prevention and treatment.
“In 15 years, drainage for SDH will likely be the most common type of adult brain surgery performed, surpassing the number of operations required for brain tumors,” Dr. Samadani said. “If we can identify patients at risk and prevent brain atrophy from occurring as Americans age, we may be able to slow this trend. If not, we are going to need increased neurosurgical and rehabilitation capacity to manage these patients.”