The classic indication for resuscitative endovascular balloon occlusion of the aorta (REBOA) is uncontrolled bleeding from known injuries to the abdomen or pelvis. But as trauma surgeons become more familiar with the techniques of endovascular resuscitation, many are exploring novel ways to use REBOA in a variety of trauma scenarios.
Recently, a team at Grant Medical Center in Columbus, Ohio, used the ER-REBOA™ from Prytime Medical to resuscitate a trauma patient in cardiac arrest from hemorrhagic shock secondary to multiple lacerations, without any truncal bleeding. According to trauma surgeon Chance Spalding, DO, PhD, the case illustrates how endovascular techniques can be combined with other interventions to treat injured patients.
Prolonged extrication with significant blood loss
The incident took place in June on a rural highway in central Ohio. A crash involving several vehicles left a young male trapped behind the wheel of a tractor-trailer. First responders spent about 2 hours extricating the driver, and the paramedics reported a large amount of blood in the cab.
“When the patient got to the ED, he was intubated and had a thready pulse that you could barely feel,” Dr. Spalding recalled. “When we exposed him, we found multiple deep lacerations in different regions of his body — the proximal thigh, the upper extremity and scalp.”
While the chief resident placed a resuscitation line in the subclavian vein, Dr. Spalding began inserting an arterial catheter in the patient’s common femoral artery. “Just as I was placing the A-line, the patient lost his pulse and went into cardiac arrest right in front of us.”
Dr. Spalding immediately up-sized the introducer sheath, prepared the ER-REBOA™ balloon and inserted the catheter. Simultaneously, the chief resident started blood transfusions while other team members performed external compressions.
“I got the balloon up into Zone 1 and inflated it — and then his heart restarted,” Dr. Spalding said. “The patient regained pulses instantaneously, and pretty soon his blood pressure was 160 systolic.”
Aortic occlusion with the ER-REBOA™ reduced the patient’s circulating volume, allowing the trauma team to concentrate on resuscitating the heart, lungs and brain. During this short period, the patient received two units of blood and two rounds of epinephrine.
“Once you verify that the heart is indeed beating and the patient has good blood pressure, you can consider taking the balloon down,” Dr. Spalding said. “That’s the hard part because this is still a very uncomfortable zone for the trauma surgeon.”
After a total occlusion time of 5 minutes, Dr. Spalding deflated the balloon. “The patient’s lacerations began bleeding again, but this showed us he had adequate blood volume and blood pressure,” he said. “We were then able to go through and quickly ligate the multiple bleeding vessels in the various lacerations. After that we did another ultrasound of the abdomen, followed by a re-examination of all the lacerations to confirm that he didn’t have any other major bleeding vessels.”
Once the patient was more stable, Dr. Spalding sent him for imaging. CT scans showed no brain trauma and confirmed no major truncal bleeding sites. “We actually got the CT while the catheter was still in place with the balloon deflated, so we were able to verify that the location was correct.”
In the ICU, the critical care team corrected the patient’s coagulopathy. “Later that evening, we pulled out the sheath and removed his endotracheal tube,” Dr. Spalding said. The patient was discharged from the hospital two days later.
A-line protocol facilitates REBOA
The trauma team at Grant trains regularly for a variety of REBOA scenarios. The team has also developed clinical protocols that support endovascular resuscitation.
“Part of our protocol for patients in hemorrhagic shock is to place a right femoral arterial line at the same time we are getting IV access,” Dr. Spalding said. This protocol facilitated an endovascular approach for the arresting patient. “We had the A-line in right away, so when the patient started to rapidly decompensate in front of us, our team was already active and ready to go with REBOA.”
Dr. Spalding noted that the AORTA trial has shown no statistical difference in time to aortic occlusion for thoracotomy with aortic cross-clamping versus REBOA. The average for each is about 6 to 7 minutes.
“For this patient, our time from ‘needle in place’ to ‘balloon up’ was about 2½ minutes, so we were well below the national average,” Dr. Spalding said. “When someone is bleeding to death, those extra minutes can make a difference.”
Important part of resuscitation toolbox
Dr. Spalding received REBOA training at Parkland Hospital in Dallas during his trauma fellowship. He also attended the Basic Endovascular Skills for Trauma (BEST) course at the RA Cowley Shock Trauma Center.
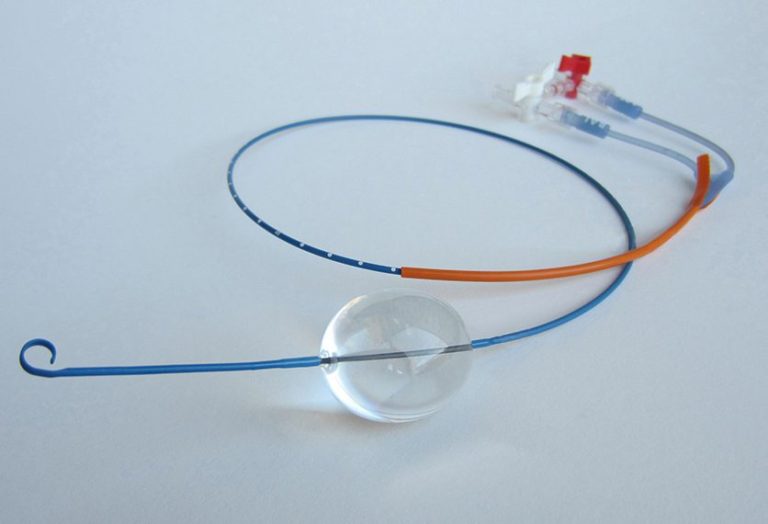
He believes the ER-REBOA™ offers several advantages in trauma scenarios. “The flexible tip reduces the risk of unwanted arterial injury, so there is more comfort with blind insertion without fluoroscopy assistance,” Dr. Spalding said. In addition, the small sheath size minimizes the chances of a local arterial complication. “For this particular patient, when I pulled the catheter out, I just held pressure on the insertion site and the patient did great.”
One big question among trauma surgeons is when exactly to deploy the ER-REBOA™. “This patient did not fit the traditional injury profile for REBOA — he exsanguinated from multiple lacerations, without any truncal bleeding,” Dr. Spalding said. “His prolonged prehospital time resulted in massive blood loss, to the point that he really lost all his circulating volume.”
“I think this case is a brilliant representation of how you can use this device as an adjunct for resuscitation,” he said. “We were able to combine REBOA with other therapies to quickly minimize the patient’s volume, circulate blood to the most critical organs, and get his heart restarted. Prior to having this device we would have had to do a thoracotomy for aortic occlusion.”
For eligible patients, REBOA offers a major benefit over resuscitative thoracotomy, Dr. Spalding noted. “Currently, the outcome between the two approaches is statistically the same — except this patient gets to go home with a needle stick in his groin instead of a large incision in his chest.”
More information for clinicians. To download instructions for the ER-REBOA™ and access other education and training information, visit Prytime Medical’s Clinical Support page.