Poor communication between nurses and physicians in a trauma surgical intensive care unit can increase the risk of adverse events. To improve SICU communication and teamwork, trauma providers at Stanford Hospital developed a nurse-driven rounding process. The new process emphasizes nursing input and leadership, structured communication and timely decision making.
The Stanford team described their implementation in a peer-reviewed report published in The Cureus Journal of Medical Science. The team launched the project in response to results from the 2014 National Database of Nursing Quality Indicators (NDNQI) Survey. In the survey, SICU nurses gave the hospital lower-than-average ratings on nurse-physician interaction, cooperation, teamwork and appreciation.
To address these issues, trauma program leaders created a task force consisting of bedside nurses, nursing leaders, attending physicians and residents. The task force focused on morning rounding as a strong opportunity to improve communication and teamwork. They developed a new rounding process based on three key changes:
1. Create a standardized rounding script
Informal surveys of SICU staff identified several weaknesses in morning rounds, including potential confusion about roles and patient orders. To prevent these communication gaps, the task force developed a standardized rounding script:
- The new script requires all team members to introduce themselves at the beginning of rounds.
- In addition to a traditional systems-based presentation from the primary resident, the new process includes a structured presentation by the bedside RN. This presentation focuses on key patient updates and staff concerns (see below for more details).
- The new process also includes real-time order entry by a resident using a mobile workstation. At the end of rounds, this resident reads back all new or modified orders.
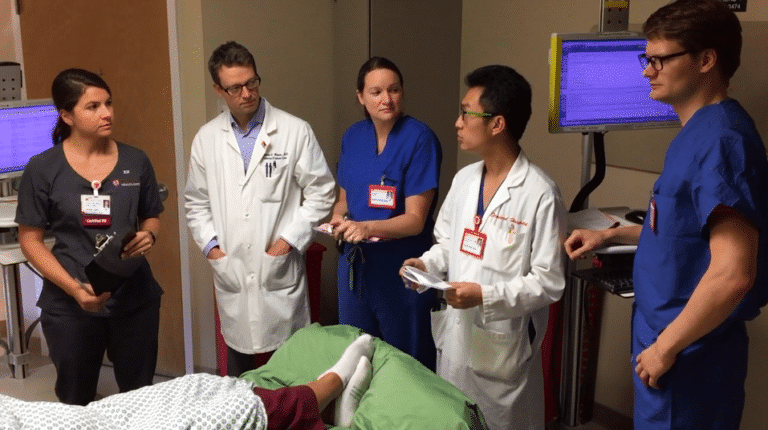
The task force created a training video that demonstrates an idealized version of their new rounding process:
https://vimeo.com/143799878
2. Give nurses a consistent leadership role
The task force also found that nursing participation in rounding was variable. While some nurses felt comfortable asking questions and providing input, others did not. To ensure a consistent role for bedside nurses, the task force developed a structured RN presentation.
Working from a template script, the bedside nurse provides updates on patient neurological, cardiac, respiratory and gastrointestinal/GU systems. The presentation also includes a patient activity report and a report of any family concerns or nursing staff issues.
According to the Trauma Performance Improvement paper, “The RN presentation was designed to give the most up-to-date clinical information, as well as to avoid the frequent situation in which the RN must correct the presenting resident with more current information, such as updated ventilator settings or drip rates.”
3. Establish a nightly check-in
The task force also found that inadequate communication during nighttime hours contributed to overall communication problems. When nighttime communication between residents and nurses was inadequate, “non-urgent issues” tended to accumulate.
To address this issue, the task force established the expectation that overnight residents perform a standardized nightly check-in. A workflow analysis identified two periods (9 p.m. to 12 midnight and 4 to 6 a.m.) as the best check-in opportunities.
“During these times, the overnight resident is expected to visit, in-person, each patient and the patient’s bedside nurse in order to address any issues or place any orders requested by the RN,” according to the TPI paper.
Implementation and outcomes
To help implement the new rounding process, the task force designated eight nurses as “SICU RN champions.” These volunteers piloted use of the RN presentation script and helped educate SICU team members on the new rounding system. They also provided feedback to the task force during the implementation period, which helped project leaders make real-time adjustments to the implementation plan as needed.
The task force used several measures to evaluate the effectiveness of the implementation. Before and after surveys showed that compliance with key elements of the rounding process increased by more than 15%. In addition, a post-implementation survey showed that nightly check-in rates were consistently above 85%.
Did the new rounding process improve team communication? Anecdotally, yes. According to the authors, several nurses and residents commented that SICU communication and working relationships had improved significantly since the new rounding process was introduced.
Survey results were less clear. As noted above, 2014 NDNQI survey results indicated significant weaknesses in SICU communication. An internal survey conducted in July 2016 using identical questions showed substantial improvement in perception of nurse-physician interactions. However, the 2016 NDNQI survey (September 2016) showed a decline in perceptions compared to 2014 results. The authors noted several factors that may account for this discrepancy, including high nursing turnover.
“Informal feedback indicated greater satisfaction among RNs and MDs with the working environment,” the authors concluded. “However, these results were not reproduced on a subsequent national survey, reflecting the difficulty of measuring intervention effectiveness using standardized surveys.”