Isolated hip fracture (IHF) is one of the most common injuries seen in trauma centers. In the U.S., 340,000 people are hospitalized for IHF every year.
These fractures typically result from low-velocity, ground-level falls, and they are a significant cause of morbidity and mortality in elderly patients. The risk of a 50-year-old woman developing an IHF during her remaining lifetime is 29%, which is higher than the risk of breast cancer, stroke or dementia.
For trauma registrars, one of the biggest challenges in abstracting an IHF chart is coding the correct procedure. It can be difficult to tell from OR reports what exactly the surgeon did and what operative approach was taken.
As always, the key to better coding is a better grasp of anatomy. Trauma registrars who understand the anatomy of the proximal femur and common hip fracture patterns will be able to code both IHF injuries and interventions more accurately.
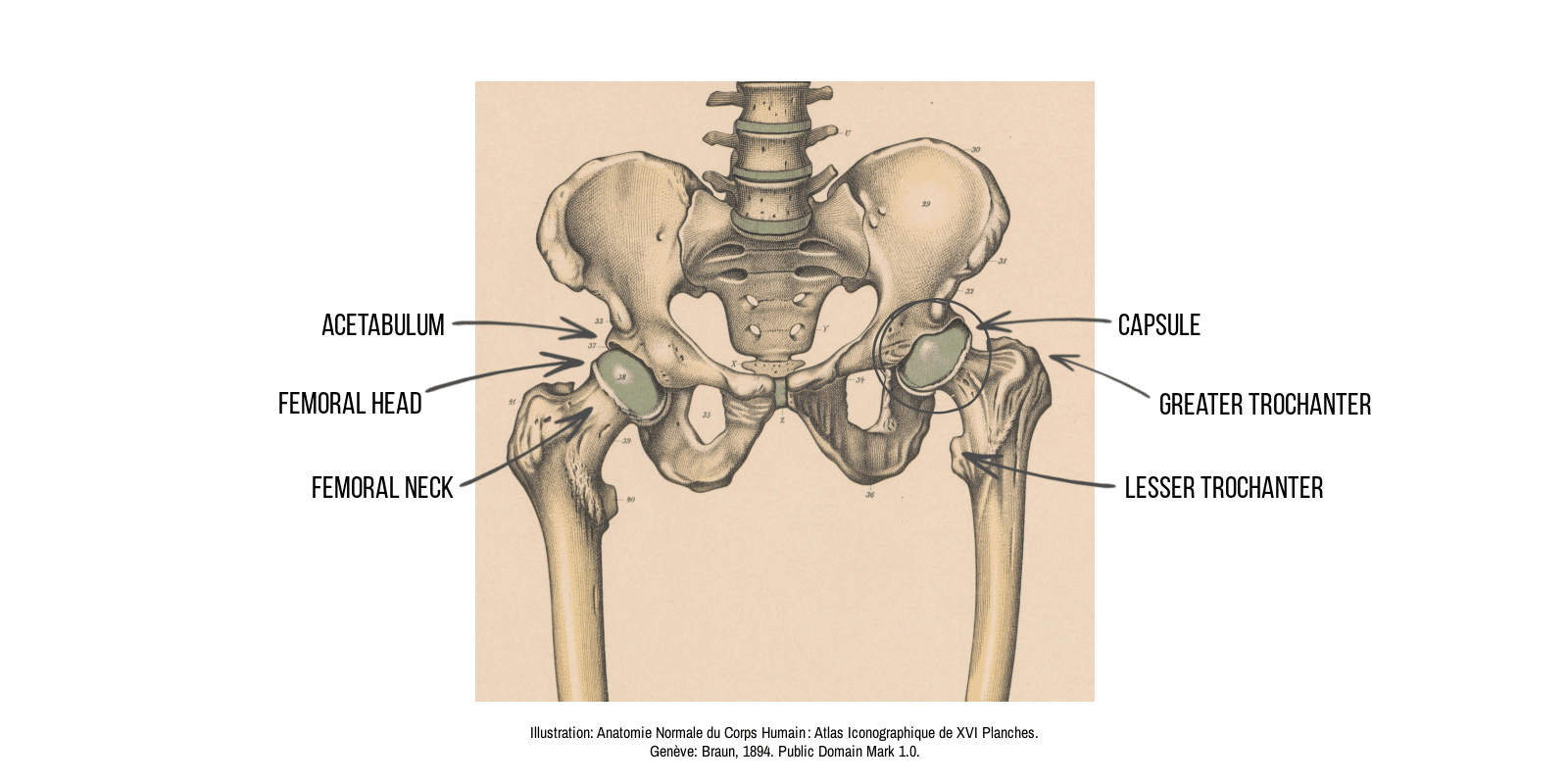
Basic anatomy of the proximal femur
To start at the most basic level, the femur is the thigh bone of the leg. The proximal femur is the end of the femur that is nearest to the body.
- The ball-shaped structure at the top of the femur is called the femoral head.
- The cup-shaped structure that the femoral head sits in is called the acetabulum.
- The narrowing under the femoral head is called the femoral neck.
- The fibrous tissue that encases the femoral head and femoral neck is called the capsule.
- The bony protrusions below the femoral neck are called the greater trochanter and the lesser trochanter.
Common isolated hip fracture patterns and typical approaches to repair
IHF typically presents as one of three common fracture types. For orthopedic surgeons, the anatomy of the fracture drives the treatment decision. The main considerations are whether the fracture occurs inside or outside the capsule, and whether or not the fracture is displaced.
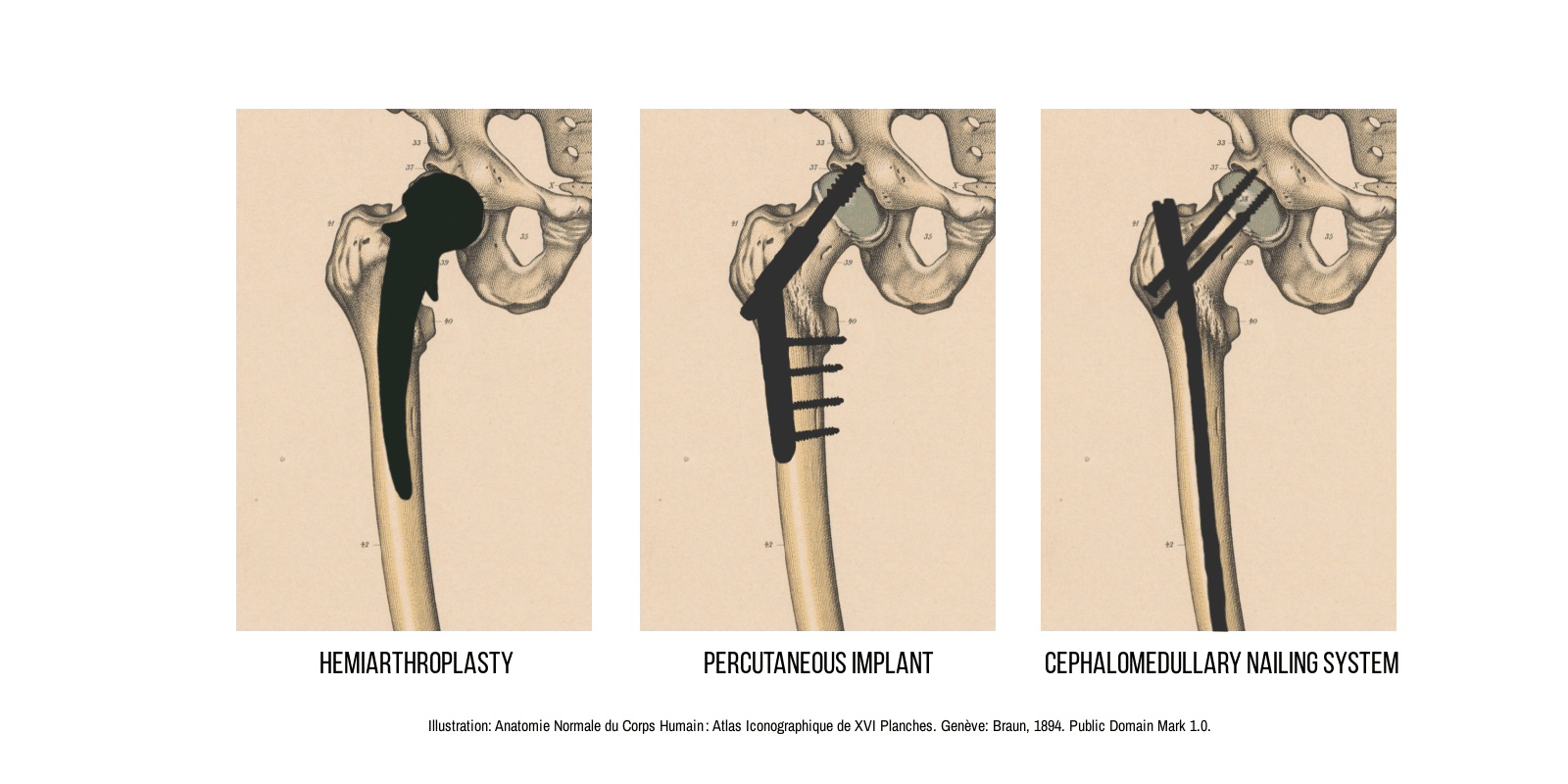
Displaced intracapsular fracture. A fracture within the capsule is typically a fracture of the femoral neck. (Fractures of the femoral head are possible but rare.)
If the femoral neck fracture is displaced, it is likely that the blood flow to the femoral head is compromised, which creates a high risk of poor healing and avascular necrosis (AVN). Approximately 9 out of 10 intracapsular fractures are displaced.
Because of the high risk of complications associated with displaced intracapsular fracture, orthopedic surgeons will almost always repair this injury with hemiarthroplasty. This procedure is essentially a hip replacement, but only the femoral head (the ball) and not the acetabulum (the socket) is replaced.
Nondisplaced intracapsular fracture. As noted above, nondisplaced intracapsular fractures are rare. These fractures carry less risk of diminished blood flow, but there is still some risk of AVN. They are usually repaired using percutaneous implants.
Extracapsular (intertrochanteric) fracture. Fractures at the level of the greater and lesser trochanters occur outside the capsule and therefore present fewer risks of complication. Extracapsular fractures heal reliably and do not have the same risk of AVN as intracapsular fractures. These fractures can typically be repaired using a cephalomedullary nailing system.
Rules to remember when coding IHF
When coding IHF, trauma registrars should keep in mind several issues and key principles:
Terminology may vary. The procedures described above are called different things by different surgeons, often depending on where they trained.
- For example, hemiarthroplasty can also be called “partial hip replacement”.
- Percutaneous implants may be referred to as various screw, pin and plate systems.
- Cephalomedullary nailing may also be known as “sliding hip screws” or “dynamic hip screws”.
We suggest working with your trauma program’s orthopedic liaison to identify the most common terminology used in your center.
Joints do not fracture in AIS. In the Abbreviated Injury Scale (AIS) scoring system, joints do not fracture. They dislocate. This means that fractures need to be coded for a bone, not a joint. Codes for IHF are found in the “Lower Extremity” chapter of the AIS Dictionary under “Proximal Femur”.
Open versus percutaneous. When coding an IHF repair in ICD-10, you will need to indicate whether the surgeon used an open approach or a percutaneous approach. To the best of our knowledge, no authoritative body has defined open versus percutaneous in terms of incision length. However, many trauma data professionals have adopted the principle that any surgical incision greater than 2 cm is an open approach and only procedures with incisions 2 cm or less are percutaneous.
Accurate IHF coding is key to a useful TQIP report
Trauma centers participating in the ACS Trauma Quality Improvement Program (TQIP) upload their data quarterly for benchmarking with like-sized facilities. Since IHF patients meet the NTDS Patient Inclusion Criteria, they are included in TQIP benchmarking reports.
TQIP includes two cohorts for IHF:
- The first IHF cohort consists of patients who are age 65 or older, whose injury mechanism is a fall, who have at least one AIS code for hip fracture (as defined in the TQIP reporting code sets), and who have no other injuries with an AIS severity between 2 and 6.
- The second IHF cohort consists of patients who have at least one of the ICD procedure codes for hip fixation.
Better IHF data leads to better patient care
Understanding the anatomy of the proximal femur, common fracture patterns and common fixation approaches will enable trauma data professionals to accurately assign codes. Trauma centers will then receive an actionable TQIP Benchmark Report and be able to determine whether the IHF patient population should be a focus for quality improvement initiatives.
References
Association for Advancement of Automotive Medicine. (2015). Abbreviated Injury Scale 2015 Dictionary. Chicago, IL: Association for Advancement of Automotive Medicine.
Rhodes H, Coile E, Eversley-Kelso T, et al. Isolated Hip Fractures in the Elderly: Best Practice Analysis of Perioperative Medical Optimization Including Effect of Comorbidities, Functional Status, and Demographics. The American Surgeon. 2022;88(8):1943-1945. doi:10.1177/00031348221091952
Optum. ICD-10-CM Expert for Hospitals: The Complete Official Code Set. Codes valid from October 1, 2022 through September 30, 2023.