Supply management is not just a cost issue. In trauma care, poorly managed supply stocks can slow down resuscitations and increase the risk of supply-related errors.
At IU Health Methodist Hospital, a Level I trauma center in Indianapolis, trauma program leaders used techniques from Lean methodology to streamline trauma supply carts, reduce supply costs and improve team efficiency.
The project was led by Catana Philipps MSN, RN, CEN, TCRN, NPD-BC, nursing professional development practitioner in the hospital’s department of trauma and acute care surgery.
Small trauma bays and poor supply management
“We had a reverification review from the American College of Surgeons in 2018,” Philipps said. “During the visit, reviewers cited our program for a weakness related to the small size of our two trauma bays.”
Each room measured 270 square feet. However, large trauma supply carts and fluid warmers consumed significant floor space, and highest-level activations were typically crowded.
Poor supply management was also an issue. “A lot of supplies were overstocked in the trauma bays,” Philipps said. “For example, we stocked a lot of extra hemostatic dressing and C-collars. We were also seeing a lot of ‘incorrect stocking’ issues being reported through our performance improvement and patients safety (PIPS) process.”
In addition, trauma supply items were not clearly labeled, making it difficult for staff to locate supplies quickly and often discouraging team members from gathering supplies proactively.
“The trauma rooms were also used for other patient populations, such as stroke and STEMI patients,” Philipps said. “We had a lot of supplies in the trauma cart — and equipment in the trauma room — that was not specific to trauma patients, so the trauma bays became a storage area for many non-emergent supplies unrelated to trauma care.”
Trauma supplies streamlined
Philipps used the Five S’s of Lean methodology to identify opportunities to eliminate unnecessary supplies from trauma bays and organize supplies for easy accessibility.
First, Philipps and trauma program manager Scott Isenberg, RN, reviewed the existing trauma carts to identify:
- Non-trauma and non-emergent items that did not need to be in the trauma bay
- Supplies only infrequently used
- Surgeon preference items no longer in use
They also assessed par levels and created new estimates (generally lower) for required stock amounts.
Next, Philipps and Isenberg used the results of their initial review to create a test cart. “We mocked up a cart and made it available to the trauma surgeons,” she said. “They actually came in and looked through the cart, then gave us feedback on items and amounts.”
As part of the trauma cart redesign, the team took a close look at chest tube supplies.
“We had a minor tray that the trauma surgeons used for chest tubes but which was also used by emergency physicians, so it not only had chest tube equipment but equipment for a few other procedures as well — 39 items in all,” she explained. “When our trauma surgeons opened the minor tray, they would have to sort through the instruments trying to figure out which ones they needed.”
Philipps and Isenberg turned to trauma medical director Peter Hammer MD, FACS, for help. “We asked which items were needed for chest tube insertion, and he gave us a list of nine items,” she said. “We then worked with sterile processing to create a new instrument tray that is now our chest tube insertion tray.”
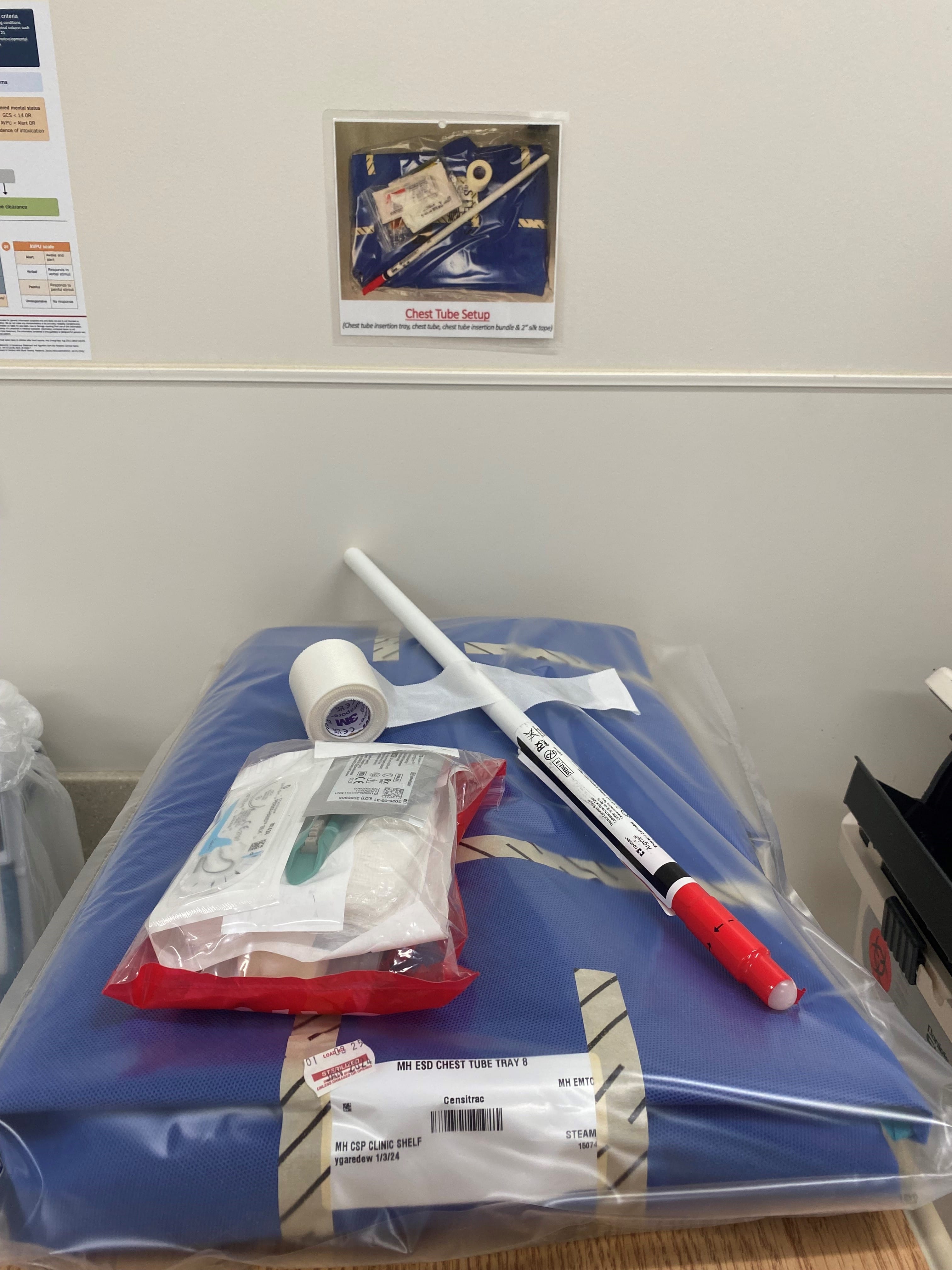
The hospital now stocks two chest tube insertion trays per room, and the minor tray is still available in the emergency department.
More space-efficient equipment purchased
To free up more space, the trauma program used budgeted funds to purchase two smaller trauma carts.

In addition, program leaders purchased eight wall-mounted fluid warmers that are also smaller than the program’s previous units.
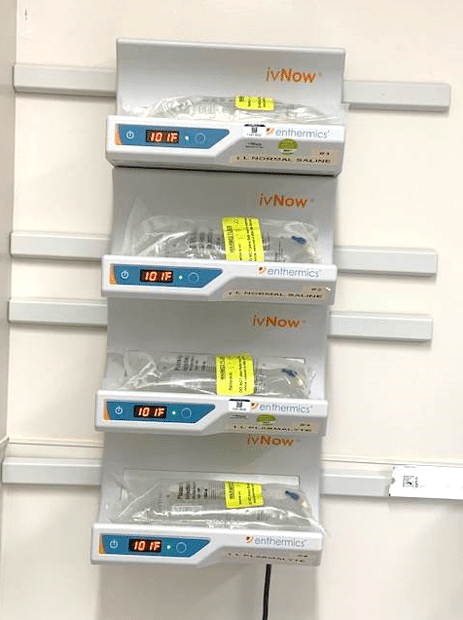
“Trauma resuscitation has evolved over the years — we have become more and more conservative with crystalloids, and we move quicker to blood,” Philipps noted. “When we looked at getting new fluid warmers, we realized we didn’t need 16 liters of fluid warmed at all times. Our new warmers hold 4 liters each, which has been a significant source of cost savings.”
Visual management introduced
Philipps also worked with the trauma team to deploy visual management strategies throughout the trauma bays. The goal was to facilitate clear communication about supplies and fast action.
“Equipment frequently moves during a trauma resuscitation or even during cleaning,” she said. “So for every piece of equipment in the trauma bay, we posted a picture on the wall showing where it goes.”
Placement photos are posted for the trauma supply cart, the defibrillator, the rapid infuser, the ventilator and other key equipment. Both trauma bays are arranged in the same way.

“We wanted to have a standardized setup so if you go in one of our trauma rooms, it’s the exact same as the one next door,” Philipps said. “Visual management allows anybody to go into a room, find the picture and know where to position a supply or piece of equipment.”
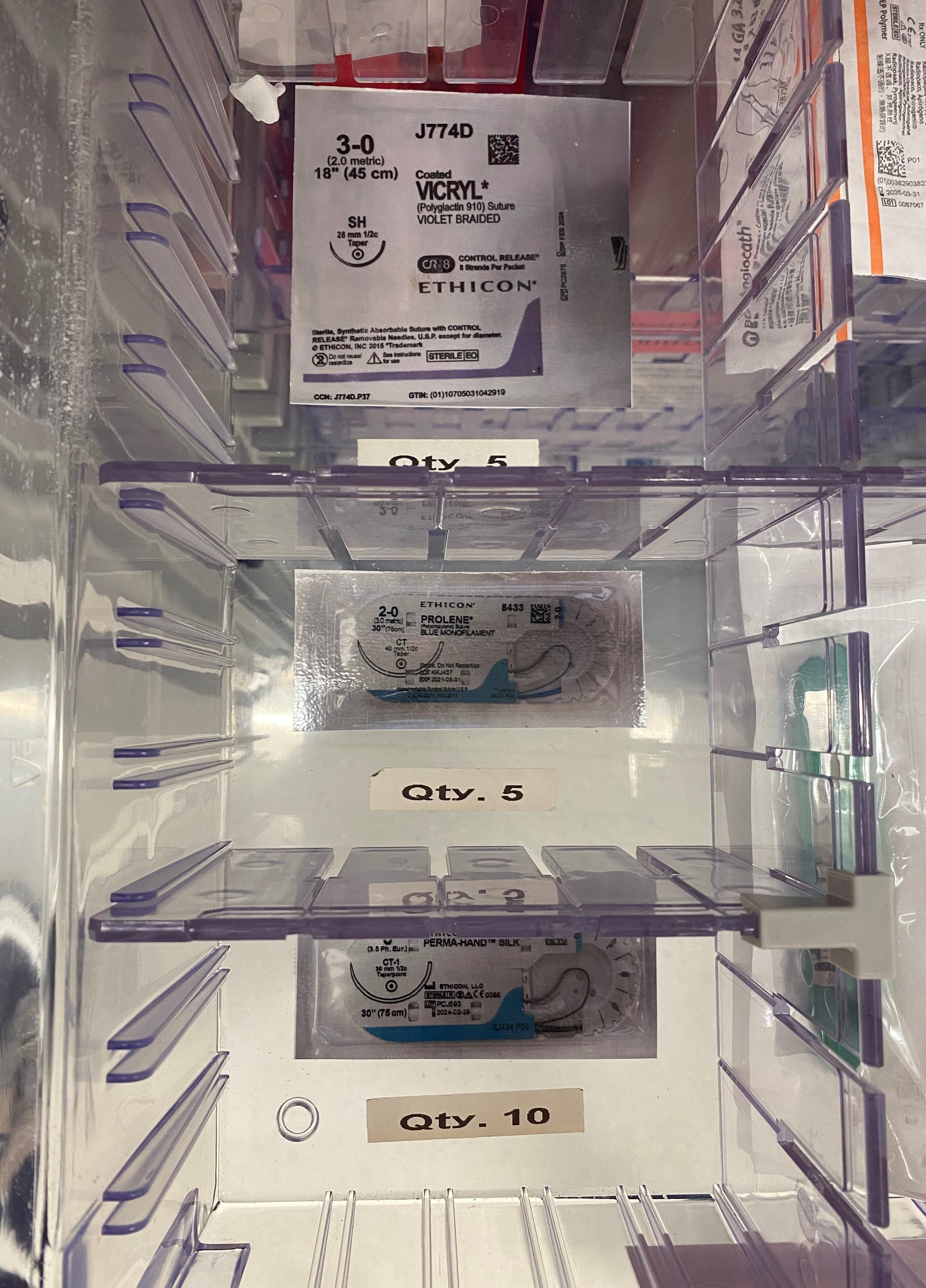
The trauma team also placed pictures of frequently mis-stocked items in trauma cart compartments.
“For example, we have a femoral arterial line kit and a radial arterial line kit, and they look identical except for a small number in the upper corner,” Philipps said. “So we took pictures of each kit, added big red circles around the size numbers, and placed each photo in the bottom of the correct compartment. Now, whoever is stocking can easily reference that photo and place the right kit in the right spot.”
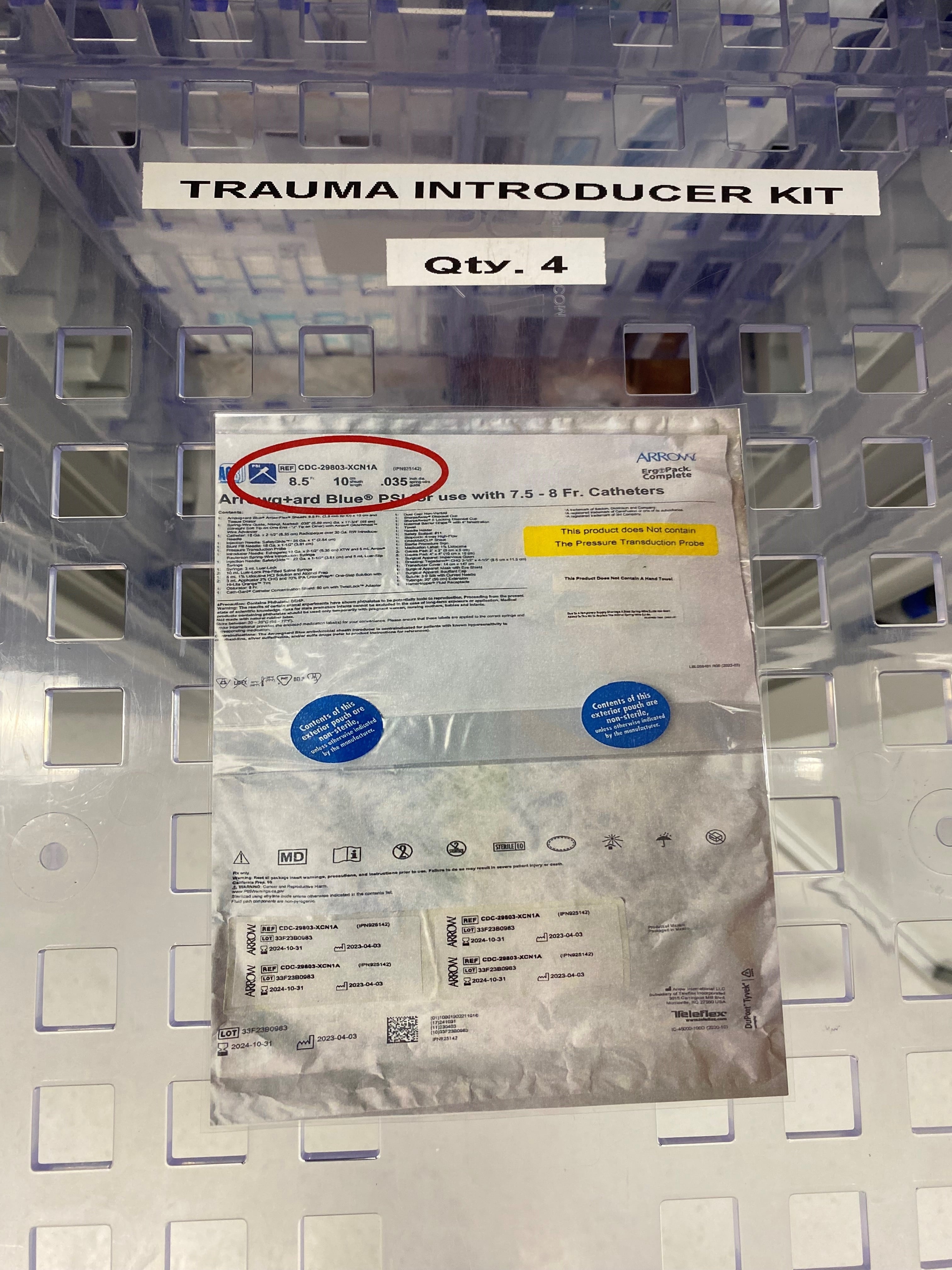
The new trauma supply carts also have clear glass doors, which increases supply visibility.
Finally, Philipps and team organized and color-coded trauma cart supplies based on the primary survey (ABCDE) — another visual reminder that helps staff access the right supplies at the right time.
Lower costs, more efficient trauma rooms
Reducing trauma cart contents not only saved space, but it also achieved financial savings.
“Our cost analysis identified a 27.4% reduction in the cost of supplies and a 79.9% reduction in the cost of intravenous fluids,” Philipps said. “All told, the total cost savings was $1,379.09 per cart.”
According to Philipps, instances of incorrectly stocked equipment reported through the trauma PIPS program have also decreased.
“Additionally, through direct observation and anecdotal feedback, we have seen that the updated trauma supply carts empower all staff members involved in trauma resuscitation to access the necessary equipment quickly,” she said.
IU Health’s trauma supply optimization project was initiated at the end of 2019, and it was implemented at the beginning of 2020. According to Philipps, the timing was fortuitous.
“We deployed these changes right before COVID started, and it turned out to be very helpful when we had to move our trauma bays into negative-pressure rooms,” Philipps said. “Since we didn’t know much about the virus at the very beginning, we had to keep our supply carts in the hallway. Having smaller carts helped a lot.”
In addition, she said the streamlining efforts proved essential: “A lot of people were redeployed from other areas, so the fact that everything was now clearly labeled made it easy for anybody to look at the cart and find what was needed.”


2 Comments
Thank you for publishing this article. I’m currently looking at decreasing costs and improving efficiency as well. Would like to see some pictures if possible.
Thanks for the suggestion, Betty. Photos added above.