Providing timely care to injured patients in Montana is a tremendous challenge. As in many rural areas worldwide, distances are vast and resources are scattered. This creates significant problems for patients who need both rapid transport to a higher level of care and immediate access to blood products.
Alyssa Johnson, MSN, RN, CEN, TCRN, helped address this problem by working with the Montana State Trauma Care Committee to choreograph a system-based response for severely bleeding patients. This effort earned the committee the 2024 Peregrine Award for Trauma Innovation in the “Level III, IV & V Trauma Centers” category.
Wake-up call
Montana is a sparsely populated state, with healthcare facilities scattered across an area of more than 147,000 square miles. According to the U.S. Census, the state’s average population density is 7.4 people per square mile, less than one-tenth the national average.
According to Johnson, who is trauma system manager for the Montana Department of Public Health and Human Services, access issues are particularly challenging for patients with severe bleeding or hemorrhagic shock.
“Many rural facilities in Montana do not have blood products readily available, and adverse weather conditions can limit air transportation options for transferring patients to major trauma centers,” Johnson explained. “This situation creates a significant challenge in providing lifesaving care to patients in rural areas who require urgent blood transfusions.”
All these issues came together in February 2019 when a 30-year-old woman suffered a ruptured ectopic pregnancy in a remote area of eastern Montana. Because of adverse weather, air transport was not an option, so the patient was loaded into a ground ambulance for a 100-mile drive to Billings Clinic. Along the way, she went into full cardiac arrest.
“Upon arrival at the trauma center, the patient received a massive transfusion protocol before undergoing surgery,” Johnson explained. “Thankfully, she made a full recovery, but this case illustrated for us the challenges of providing blood to patients in our rural communities.”
What is possible?
Since an MTP had been activated, the case was reviewed by the blood utilization committee at Billings Clinic from a performance improvement perspective.
“The committee recognized that the ambulance drove right by another hospital that might have had blood,” Johnson said. “So they asked, Could the patient have gotten blood at that hospital? But then other questions came up: Did that hospital actually have blood? If it did have blood, how would other providers know?”
The first step to answering all these questions was to develop a statewide map of existing blood resources. Montana is served by two different blood suppliers, the American Red Cross and Vitalant. The map plots out which facilities are supplied by which organization (see below).
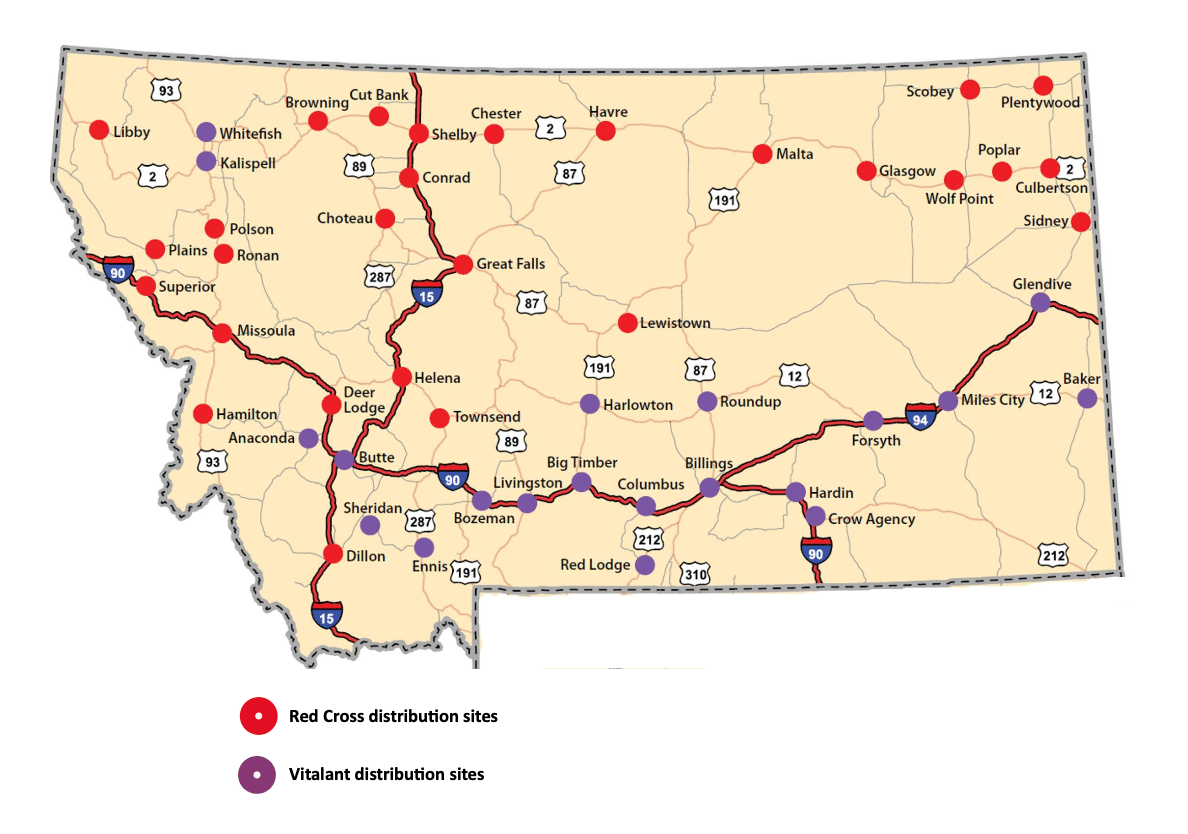
Initially, the blood resource map also covered northern Wyoming, which is within the catchment area for Billing Clinic. “The map later became Montana-centric,” Johnson explained, “because we learned that according to federal law, blood cannot cross state lines without the appropriate licensing.”
The next step was to determine whether hospitals in the state were open to the concept of sharing blood products with patients being transported between two other facilities. While the index case that started this effort was not a trauma patient, state health leaders realized that the Montana State Trauma Care Committee was the logical choice to tackle this challenge.
The committee began by distributing a survey questionnaire to trauma coordinators and healthcare providers across Montana. The survey was designed to gauge interest in a blood-sharing system and identify potential barriers to implementation.
“The results demonstrated strong support for the basic concept, with 92.5% of respondents agreeing that ambulances should be able to pick up blood products from intermediary facilities for transfusion during transport,” Johnson said.
Clear guidelines
The survey was administered in January 2020, so work on the blood-sharing initiative was soon brought to a halt by the COVID-19 pandemic. Finally, in April 2022, the Montana State Trauma Care Committee approved and launched the Montana Interfacility Blood Network (MT-IBN).

“The MT-IBN is a novel concept that enables healthcare facilities to support each other in times of need, overcoming the logistical hurdles posed by Montana’s remote geography,” Johnson said. “Essentially, if a patient presents at a rural facility with no or limited blood supplies — and air transport is grounded due to weather — the ground ambulance can pick up un-crossmatched, emergent blood products from an intermediary facility along the transport route.”
As part of MT-IBN implementation, the Montana State Trauma Care Committee developed a comprehensive set of guidelines and implementation resources, including:
Guidelines for sharing blood. Only Type O blood is given within the network’s hand-off system. “No historical blood types or verbal blood types can be honored,” Johnson said. “This is emergent release blood only.”
Blood sharing processes. (1) The sending facility determines that a patient will require blood en route to a higher level of care. (2) The sending facility notifies the receiving facility that the patient is coming and that the ambulance will be picking up blood along the way. (3) The sending facility contacts the intermediary facility to arrange the blood release and the logistics of the hand-off.
Required resources and staff. In addition to blood products, tubing and other supplies, qualified staff must be available to administer blood during transport. “In Montana, that must be a paramedic, a critical care paramedic, an RN or a medical provider,” she said. “A lot of facilities in our state only have BLS available, so it is not uncommon to put a nurse or a doctor in the back of the ambulance during a long transport.”
Blood packaging guidelines. Proper packaging is key to avoiding waste. The blood packaging guidelines from the American Red Cross and Vitalant are similar but they have specific differences.
Required documentation. Proper transfer documents (again, for the correct blood supplier) must accompany all blood products shared within the MT-IBN.
Resupply and billing processes. Resupply was a key issue for participants, because some facilities in the state have only two units on hand at any given time. “Under the guidelines, the facility that shares the blood is responsible for immediately notifying their supplier to arrange for resupply,” Johnson said.
“For blood products that are transfused en route, compatibility testing and charging occurs at the receiving facility,” she added. If the blood products do not end up being transfused, they can be brought into the receiving facility’s blood bank as long as they are packaged appropriately, even if they are sent from a different supplier. “Alternatively, if the ambulance is going back to the community, the blood products can be brought back to the intermediary facility — again, as long as they are packaged appropriately.”
According to Johnson, law enforcement plays an important role in the MT-IBN. “It is not uncommon for the State Highway Patrol to pick the blood up at the intermediary hospital and ferry it to a transfer point,” she said. “That way, the ambulance doesn’t need to exit the highway and drive all the way to the sharing hospital. They may just need to pull off to the side of the road for a minute or two.”
Does this system violate emergency treatment laws? “We are often asked whether this violates EMTALA,” Johnson said. “The answer is no — because the ambulance is not stopping for an evaluation, it is simply stopping for a resource. So the patient does not need to be registered or evaluated at the intermediate facility.”
Cooperation in voluntary network
“The uniqueness of the MT-IBN stems from the cooperation it fosters between dozens of independent hospital systems and small critical access facilities across the state,” Johnson said. “Since its implementation, the system has been activated for several patients. In addition, the voluntary network has grown rapidly as many rural hospitals have recognized its potential to save lives.”
Johnson and colleagues authored a paper on the creation and implementation of the Montana Interfacility Blood Network. “The Montana Interfacility Blood Network: A Novel Lifesaving “Hand-off” for the Optimal Care of Rural Patients” was published in the March 2024 issue of the Journal of Blood Medicine.
Learn more
Johnson talked about the Montana Interfacility Blood Network in detail during the May 2024 online event honoring the winners of the Peregrine Award for Trauma Innovation. To view the webinar on-demand, visit Profiles in Trauma Innovation: Improving Trauma Data Quality and Trauma System Collaboration.