The American College of Surgeons requires trauma programs to monitor patient care and system processes on a continuous basis using a reliable method of data collection. This is where the words “track and trend” come into play. The problem is that using data to monitor trauma team performance can be very challenging.
For example, if you have two OR delays in July and three in August, does that mean your trauma team’s performance is slipping? If you have two undertriage events in September and none in October, does that mean your performance is improving?
In spite of our best efforts to analyze performance improvement (PI) data correctly, the numbers can easily be unclear or even misleading.
My search for data-driven PI
When I was the trauma program manager at a Level II pediatric trauma program, I struggled to find tools for identifying performance trends and evaluating whether our PI program was effective while being efficient.
A bar graph or line chart seemed like the logical choice for monitoring performance, but I soon learned that these tools have a major weakness: They do not take into account fluctuations in patient volume and acuity.
For example, say you are monitoring ventilator associated pneumonia (VAP) by plotting the number of VAP cases each month in a line graph. If the number of cases dips one month, you might deduce that the numbers are improving. However, the line graph is not taking into account the actual number of intubated patients. The dip you saw may be during a month with a low volume of ventilated patients, rendering the chart useless as a performance monitoring tool.
I also learned that percentages are not the solution. The underlying statistics here are little more complex, but the basic problem goes back to sample size and common variation in data. For issues that occur less frequently, it is impossible to tell whether a percentage fluctuation is driven by a true PI problem or some other factor.
What’s the answer? About two years ago, I was introduced to statistical process control (SPC) by Genie Roosevelt, MD, MSPH, associate professor of emergency medicine at the University of Colorado School of Medicine.
SPC is the methodology of choice in the manufacturing industry for measuring and controlling quality, but it is also incredibly useful in healthcare. Why? Because it helps us distinguish between common cause variation (expected, normal variation in data) and special cause variation (which represents a statistically significant change in process). In other words, SPC lets us separate the signal from the noise.
A chart for all seasons
SPC encompasses dozens of tools and processes, but there is one tool that I turn to more frequently than any other — the P chart.
A P chart is a type of control chart that uses proportions to determine whether variation in data is significant. You can use a P chart retrospectively to determine whether a PI initiative was successful. You can also use P charts to monitor patient care or system issues on a concurrent, continuous basis.
But isn’t SPC complicated? The answer is yes. However, with the advent of new software widely available to the public, the rigorous statistical mathematics associated with SPC can be computed “behind the scenes.”
Using a P chart is one of the easiest way to get started with SPC. It’s also a great tool for achieving strong results quickly in your PI program. Here is my five-step process for using a P chart to monitor trauma performance improvement.
1. Make sure a P chart is right for your project
I recommend P charts to all my trauma colleagues. However, SPC includes several other kinds of control charts for monitoring performance. I would be remiss if I did not mention that choosing the correct control chart is essential to gaining accurate and meaningful information from SPC.
There are several ways to select a control chart. The easiest is to use the automated process embedded in your SPC software. The software I use is QI Macros, an Excel add-on. QI Macros features a “Chart Wizard” function — you just plug in your data and the software determines which kind of chart is right for your needs.
You can also refer to an SPC decision tree. Here’s a control chart decision tree available from QI Macros. Alternatively, search for “control chart decision tree” online and you will find several good options.
The basic decision comes down to two questions:
- Is your sample size constant or variable? (For most things you might want to track in healthcare, sample size will be variable, since patient volume is constantly changing.)
- Will you be measuring continuous data or attribute data? (Continuous data refers to “continuous scale” measures like height, weight and time. Attribute data refers to yes/no measures or counting data such as number of admissions, number of undertriages, number of late attending arrivals, etc.)
If you have attribute data with a varying sample size, a P chart is most likely what you should use.
2. Gather your data
P charts work by monitoring the proportion of nonconforming units in a sample. So in the data gathering phase, you will be tracking (a) the sample and (b) the nonconforming units.
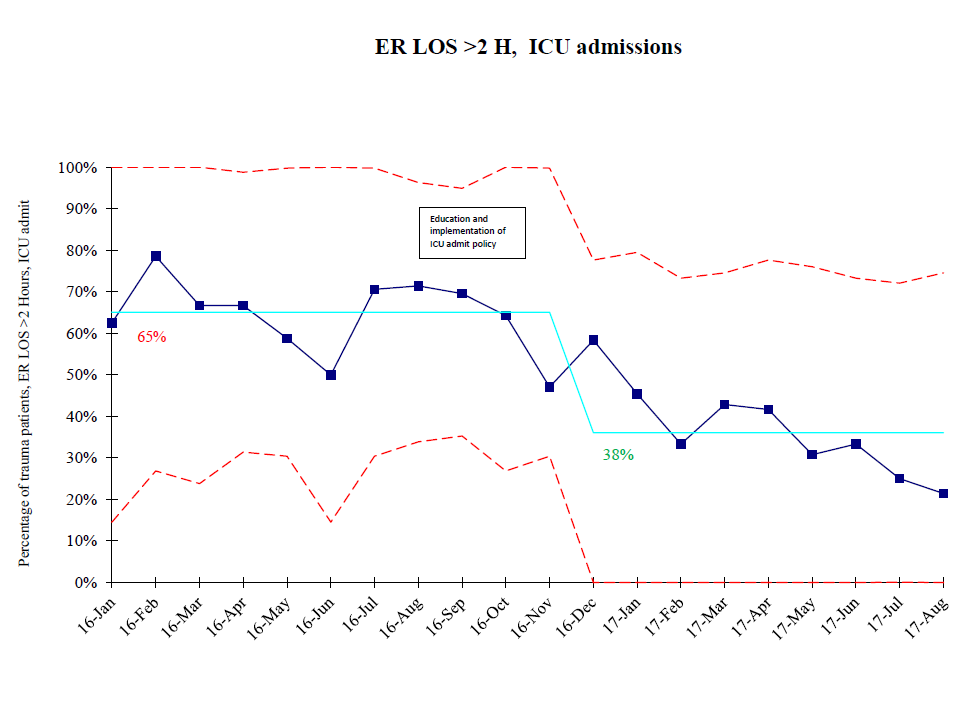
For example, like all trauma teams, my colleagues and I want to make sure critically ill trauma patients are rapidly triaged out of the emergency room to their inpatient destination. To do this, one thing we monitor is ER length-of-stay for patients admitted to the ICU. For this process, the sample is all ICU admissions in the emergency department. We define the nonconforming unit as any ICU admission with an ER length-of-stay greater than 2 hours.
The sample can be monthly, quarterly or yearly depending on volume and the process being monitored. The less common an issue or process, the larger a time period you will require for sampling.
3. Plug in your numbers
Once you collect data on your nonconforming units and your sample, enter this data in the appropriate columns in your software.
For example, you might be using a P chart to monitor undertriage. In this case, your nonconforming units could be patients with an ISS >15 with limited or no activation. The sample would be the number of patients with an ISS >15. Again, the sample could be monthly, quarterly or longer depending on demographics of your trauma program.
Once your data is entered into the program, your software will generate the P chart. In QI Macros, I use the P chart template provided in the software. I find that using the template makes data entry and chart production less cumbersome.
4. Use the chart to identify “special cause variation”
Your P chart will show the performance data plotted over time, a center line and control limits. The center line is the average of the data. The upper and lower control limits are usually ±3 standard deviations of the plotted statistic from the mean.
The control limits are what differentiate a P chart from a simple line graph. They are essential to determining whether there is common cause variation or special cause variation in data. In other words, you use the control limits to determine whether your team’s performance is getting better, getting worse or holding steady.
To do this, examine the data points on the P chart and look for specific patterns, for example:
- 1 point above or below the upper or lower control limit
- 8 consecutive points above or below the center line
- 6 consecutive points steadily increasing or decreasing
There are several other patterns that indicate a statistically significant change in process. You can learn them all or simply use your software to analyze the data points for you. For example, QI Macros has the ability to run a stability analysis. This function will highlight any special cause variation, alerting you to any statistically significant process change, either good or bad.
For instance, say your PI process is focusing on timely arrival of attending surgeons. You are using a P chart to track attending arrival times, and the chart shows 8 consecutive points below the center line. This lets you know that there has been a significant shift in performance. In this case, points below the center line indicate that attending arrival times have decreased and PI efforts have been successful.
For another example, let’s return to my team’s ER length-of-stay monitoring (see our chart at right). As you can see, special cause variation adjusts the center line to reflect the new average. One takeaway from this is that if the chart shows a process is in control and the average is moving in the right direction, you know that your performance is improving.
5. Understand the issues and fix any problems
Of course, control charts do not just deliver good news. What happens when your P chart indicates worsening performance?
When a P chart identifies special cause variation indicating that either a process is out of control or performance is worsening, it is time to take a deep dive into the patient care or system issue you are monitoring.
Let’s say our ED length-of-stay was getting longer for ICU admits. The first step is to investigate the issues. Are there new nurses in the emergency department? Are there new residents? Is the increased wait time related to volume? Is it driven by bed capacity?
When you think you have identified the barrier, your PI team can plan and implement a correction. The same chart can then be used to monitor your intervention for either success or failure.
Take PI to the next level
Used appropriately, a P chart gives you the ability to focus on statistically significant trends and not react to common variation in data. It is a powerful tool that can take your trauma PI program to the next level and help you ensure safe, timely and effective patient care.
Megan Hiser, MSN, RN is director of trauma quality and analytics at HCA Continental Division. She can be reached at megan.hiser424@gmail.com.

